Cesarean
A cesarean delivery (also called a surgical birth) is a surgical
procedure used to deliver an infant . It requires
regional (or rarely general) anesthetic to prevent pain, and then a vertical or
horizontal (‘bikini line’) incision in the lower abdomen to expose the uterus
(womb). Another incision is made in the uterus to allow removal of the baby and
placenta. Other procedures, such as tubal ligation (sterilization), may also be
performed during cesarean delivery.
REASONS FOR CESAREAN DELIVERY
Some women who intend to deliver vaginally will
eventually require cesarean delivery. The following list describes some reasons
cesarean might be needed:
- Labor is not progressing as it
should. This may occur if the contractions are too weak, the baby is too
big, the pelvis is too small, or the baby is in an abnormal position. If a
woman's labor does not progress normally, in many cases, the woman will be
given a medication (Pitocin/oxytocin) to be sure that
contractions are adequate for several hours. If labor still does not
progress after several hours, a cesarean delivery may be recommended.
- The baby's heart rate suggests
that it is not tolerating labor well.
- The baby is in a transverse
(sideways) or breech position (buttocks first) when labor begins.
- Heavy vaginal bleeding. This
can occur if the placenta separates from the uterus before the baby is
delivered (called a placental abruption).
- A medical emergency threatens
the life of the mother or infant
PLANNING CESAREAN
DELIVERY
A planned cesarean delivery is one that is
recommended because of the increased risk(s) of a vaginal delivery to the
mother or her infant. Cesarean deliveries that are done because the woman
wants, but does not require, a cesarean delivery are called
"maternal request cesarean deliveries". (See 'Maternal request cesarean delivery' below.)
There are a number of medical and obstetric
circumstances that a healthcare provider would recommend scheduling a cesarean
delivery in advance. Some of these circumstances are listed below:
There is some controversy about the preferred
method of delivery in certain situations. These include some birth defects,
such as spina bifida and fetal abdominal wall defects, and some maternal
medical problems.
One of the most important factors in scheduling
a cesarean delivery is making certain that the baby is ready to be delivered.
In general, cesarean deliveries are not scheduled before the 39th week of
pregnancy. An amniocentesis may be recommended to determine if the baby's lungs
are fully developed, especially if cesarean is planned before 39 weeks of
pregnancy.
Most women will meet with an anesthesiologist
before planned surgery to discuss the various types of anesthesia available and
the risks and benefits of each. Instructions about how to prepare for surgery
will also be given, including the need to avoid all food and drinks for 10 to
12 hours before the surgery.
Advantages of planned cesarean — The advantages of a planned cesarean delivery
include:
- It allows parents to know
exactly when the baby will be born, which makes issues related to work,
childcare, and help at home easier to address.
- It avoids some of the possible
complications and risks to the baby.
- It avoids the possibility of
postterm pregnancy, in which the baby is born two or more weeks after its
due date.
- It helps ensure that a pregnant
woman's obstetrician will be available for the delivery.
- It may offer a more controlled
and relaxed atmosphere, with fewer unknowns such as how long labor and
delivery will last.
- It may minimize injury to the
pelvic muscles and tissues and the anal sphincters. These injuries
sometimes occur during vaginal delivery, which may increase the risk of
urinary or anal incontinence.
The benefits of planned cesarean delivery must
be weighed against the risks. Cesarean delivery is a major surgery, and has
associated risks.
Risks — Because
cesarean delivery involves major surgery and anesthesia, there are some
disadvantages compared to vaginal delivery.
- Cesarean delivery is associated
with a higher rate of injury to abdominal organs (bladder, bowel, blood
vessels), infections (wound, uterus, urinary tract), and thromboembolic
(blood clotting) complications than vaginal delivery.
- Cesarean surgery can interfere
with mother-infant interaction in the delivery room.
- Recovery takes longer than with
vaginal delivery.
- Cesarean delivery is associated
with a higher risk that the placenta will attach to the uterus abnormally
in subsequent pregnancies, which can lead to serious complications.
- Cutting the uterus to deliver
the baby weakens the uterus, increasing the risk of uterine rupture in
future pregnancy. This risk is small and depends upon the type of uterine
incision.
Infant risks — There
are few risks of cesarean delivery for the infant. One risk is birth trauma,
which is rare. Temporary respiratory problems are more common after cesarean
birth because the baby is not squeezed through the mother's birth canal. This
reduces the reabsorption of fluid in the infant's lungs.
Potential complications — The most common complications related to cesarean
delivery include infection, hemorrhage (excessive bleeding), injury to pelvic
organs, and blood clots.
- Infection — The risk of
postoperative uterine infection (endometritis) varies according to several
factors, such as whether labor had started and whether the water was
broken. Endometritis is treated with antibiotics.
Wound infection, if it occurs, usually develops
four to seven days after surgery, but sometimes appears during the first day or
two. In addition to antibiotics, wound infections are sometimes treated by
opening the wound to allow drainage, cleansing with fluids, and removing
infected tissue if needed.
- Hemorrhage — One to two percent
of all women having cesarean deliveries require a blood transfusion
because of hemorrhage (excessive bleeding). Hemorrhage usually responds to
medications that cause the uterus to contract or procedures to stop the
bleeding. In rare cases, when all other measures fail to stop bleeding, a
hysterectomy (surgical removal of the uterus) may be required.
- Injury to pelvic organs —
Injuries to the bladder or intestinal tract occur in approximately one
percent of cesarean deliveries.
- Blood clots — Women are at
increased risk of developing blood clots in the legs (deep vein thrombosis
or DVT) or the lungs (pulmonary embolus) during pregnancy and the
postpartum period. This risk is further increased after cesarean delivery.
The risk can be reduced by using a device that gently squeezes the legs
during and after surgery, called an intermittent compression device. Women
at high risk of DVT may be given an anticoagulant (blood thinning)
medication to reduce the risk of blood clots.
MATERNAL REQUEST
CESAREAN DELIVERY
The concept of requesting a cesarean delivery is
relatively recent. In the United States and most Western countries, pregnant
women have the right to make choices regarding treatment, including how they
will deliver their child.
A woman who wants to request a cesarean delivery
should discuss this decision with her healthcare provider. He or she can
provide information about each method of delivery and can help to relieve
common fears about pain, the expected process of labor, as well as the woman's
right to determine how she will deliver. The woman should also discuss the
risks and benefits of maternal request cesarean delivery; in general, the risks
are the same as those of a planned cesarean delivery. The woman should also
discuss the possible need for a cesarean delivery with future pregnancies.
Regardless of a woman's decision, it is possible
to reconsider the decision at any time based upon a change in circumstances.
EMERGENCY CESAREAN
DELIVERY
In some cases, cesarean delivery is performed as
an emergency surgery, after attempting a vaginal delivery. Time may be of the
essence, depending upon the situation. Cesarean deliveries performed due to
concerns about the mother's or infant's health are started as quickly as
possible.
In contrast, if a cesarean is performed because
labor has not progressed normally or for other, less serious concerns about the
baby's wellbeing, the surgery is usually begun within 30 to 60 minutes.
If an epidural was placed before the attempted
vaginal delivery, it can be used to administer anesthesia for the cesarean
delivery (a larger dose is necessary for cesarean delivery versus vaginal
delivery). Otherwise, spinal anesthesia (or rarely general anesthesia) is
given.
After being admitted to the hospital, a woman
may be given an oral dose of an antacid to reduce the acidity of the stomach
contents. Another medication may be given to reduce the secretions in the mouth
and nose. An intravenous line will be placed into the hand or arm, and an
electrolyte solution will be infused. Monitors will be placed to keep track of
blood pressure, heart rate, and blood oxygen levels.
Anesthesia — The
woman is usually accompanied to an operating room before anesthesia is
administered. A spouse or partner can usually stay with the woman in the
operating room.
There are two types of anesthesia used during
cesarean delivery: regional and less commonly, general. For a planned cesarean
delivery, regional anesthesia is usually performed. Meeting with the
anesthesiologist allows the woman to ask specific questions about anesthesia,
and allows the anesthesiologist to identify any medical problems that might
affect the type of anesthesia that is recommended.
With epidural and spinal anesthesia, the
anesthetic is injected near the spine, which numbs the abdomen and legs to
allow the surgery to be pain-free while allowing the mother to be awake.
General anesthesia induces unconsciousness. This
means that the mother will not be awake or aware during the procedure. After
the anesthesia is given, the woman will fall asleep within 10 to 20 seconds and
a tube will be placed in the throat to assist with breathing. General
anesthesia carries a greater risk of complications than epidural or regional
anesthesia because of the need for an endotracheal (breathing) tube and because
drugs given to the mother affect the infant.
Women who have general anesthesia will not be awake during the cesarean
delivery. Regional anesthesia is generally preferred because it allows the
mother to remain awake during the procedure, enjoy support from staff and a
family member, experience the birth, and have immediate contact with the
infant. It is usually safer than general anesthesia.
After the anesthesia is given, a catheter is placed
in the bladder to allow urine to drain out during the surgery and reduce the
chance of injury to the bladder. The catheter is usually removed within 24
hours after the procedure.
Skin incision — There
are two basic types of incision: horizontal (transverse or "bikini
line") and vertical (midline). Most women have a transverse skin incision,
which is made 1 to 2 inches above the pubic hair line. The advantages of this
type of incision include less postoperative pain, more rapid healing, and a
lower chance that the wound will separate during healing.
Less commonly, the woman will have a vertical
("up and down") skin incision in the midline of the abdomen. The
advantages of this type of incision include rapid access to the uterus (eg, if
the baby is in distress or if the woman is bleeding excessively).
Uterine incision — The uterine incision can also be either transverse or
vertical. The type of incision depends upon several factors, including the
position and size of the fetus, the location of the placenta, and the presence
of fibroids. The main consideration is that the incision must be large enough
to allow delivery of the fetus without causing trauma.
The most common uterine incision is transverse.
However, a vertical incision may be required if the baby is breech or sideways,
if the placenta is in the lower front of the uterus, or if there are other
abnormalities of the uterus.
After opening the uterus, the baby is usually
removed within seconds. After the baby is delivered, the umbilical cord is
clamped and cut and the placenta is removed. The uterus is then closed. The
abdominal skin is closed with either metal staples or reabsorb able sutures.
After the mother and baby are stable, she or her
partner may hold the baby.
After surgery is completed, the woman will be
monitored in a recovery area. Pain medication is given, initially through the
IV line, and later with oral medications.
When the effects of anesthesia have worn off,
generally within one to three hours after surgery, the woman is transferred to
a postpartum room and encouraged to move around and begin to drink fluids and
eat food.
Breastfeeding can usually begin anytime after
the birth. A pediatrician will examine the baby within the first 24 hours of
the delivery. Most women are able to go home within three to four days after
delivery.
Staples are usually removed within three to
seven days of delivery, while reabsorbable sutures are absorbed by the body and
do not need to be removed.
The abdominal incision will heal over the next
few weeks. During this time, there may be mild cramping, light bleeding or
vaginal discharge, incisional pain, and numbness in the skin around the
incision site. Most women will feel well by six weeks postpartum, but numbness
around the incision and occasional aches and pains can last for several months.
After going home, the woman should notify her
healthcare provider if she develops a fever (temperature greater than 100.4º F
[38º C]), if pain or bleeding worsens, or there are other concerns.
Previously, obstetricians recommended that all
women who had a cesarean delivery have the same for all future deliveries.
However, this is no longer the case. Most women in the United States who have
had one low transverse cesarean delivery choose to have a repeat cesarean
delivery, although these women could try to have a vaginal delivery with the
next pregnancy. Between 60 and 80 percent of women who try to deliver vaginally
after a c-section are successful in delivering vaginally. However, women who
have a vaginal birth after cesarean (VBAC) have a less than 1 percent chance
that the uterus will rupture during delivery, which could affect the baby's
health .
WHERE TO GET MORE
INFORMATION
Your healthcare provider is the best source of information
for questions and concerns related to your medical problem.
This article will be updated as needed on our
web site (www.uptodate.com/patients). Related topics for
patients, as well as selected articles written for healthcare professionals,
are also available. Some of the most relevant are listed below.
Patient level information — UpToDate offers two types of patient education
materials.
The Basics — The
Basics patient education pieces answer the four or five key questions a patient
might have about a given condition. These articles are best for patients who
want a general overview and who prefer short, easy-to-read materials.
Beyond the Basics — Beyond the Basics patient education pieces are
longer, more sophisticated, and more detailed. These articles are best for
patients who want in-depth information and are comfortable with some medical
jargon.
Professional level information — Professional level articles are designed to keep
doctors and other health professionals up-to-date on the latest medical
findings. These articles are thorough, long, and complex, and they contain
multiple references to the research on which they are based. Professional level
articles are best for people who are comfortable with a lot of medical terminology
and who want to read the same materials their doctors are reading.
C
Section Recovery
By section recovery
10 common questions
about C Section Recovery
1. How long is the C Section
Recovery time?
Generally, you will feel better within 2 weeks but it takes another 4 weeks to
heal your wound. That’s why the doctors say about 6 weeks.
2. How long does the pain last for?
You can expect to be very sore for several days, upto 2 weeks. Standing
straight will be very difficult too. You do experience burning or a pulling
sensation when standing or walking around.
3. What aggravates the pain?
Coughing, sneezing, and laughing will make it very painful. Getting up to walk
will also be painful but you have to do it. You must walk LOTS to stimulate
circulation and encourage the healing.
4. What do I do with swollen feet?
Keep your feet elevated while resting. And rest often.
5. Can I climb up stairs?
It is not recommended to go up stairs. It would be better to move temporarily
to the common area for a week or two. But if you have to climb stairs, do it
very slowly and hold onto the handles.
6. How do I care for my wound?
Clean and Sterilise your wound. Your wound must be kept dry and clean to avoid
infection. Use a mirror to monitor the wound.
Warning signs of infection are : oozing from the incision, if you have high
fever of 100 degrees or higher, foul smell from incision, redness and pain at
the incision.
7. Can I do lifting or exercises?
You cannot lift anything heavier than your baby. And the only exercise you
should be doing is walking and pelvic tilt exercises.
Mistakenly, as soon as a mother ‘feels better’, they have this energy burst and
they feel like cleaning and tidying up. But quite often, pain returns again and
in some cases, infection in the incision occurs – and that is extremely
painful.
8. When can I drive again?
After 2-3 weeks
9. What do I do with my active preschooler?
From toddler age, your child can understand what you tell them if you explain
what has happened in simple words. That is, your tummy is too sore to pick them
up but you could have a cuddle together. Also, a good icebreaker is to buy a
gift for your toddler and say it is from the baby when you arrive back home.
10. How do I recover faster?
If you want a faster C Section recovery with less pain, less stretch marks, less
visible scar, you need to support yourself with an abdominal
binder. The binder will
support your posture while you’re breastfeeding, it will reduce the pain you as
you get up to walk and it will protect your incision from infection. If you buy
the C Section Recovery Kit, it will show you how to reduce your scarring to
virtually invisible. You deserve to be looked after
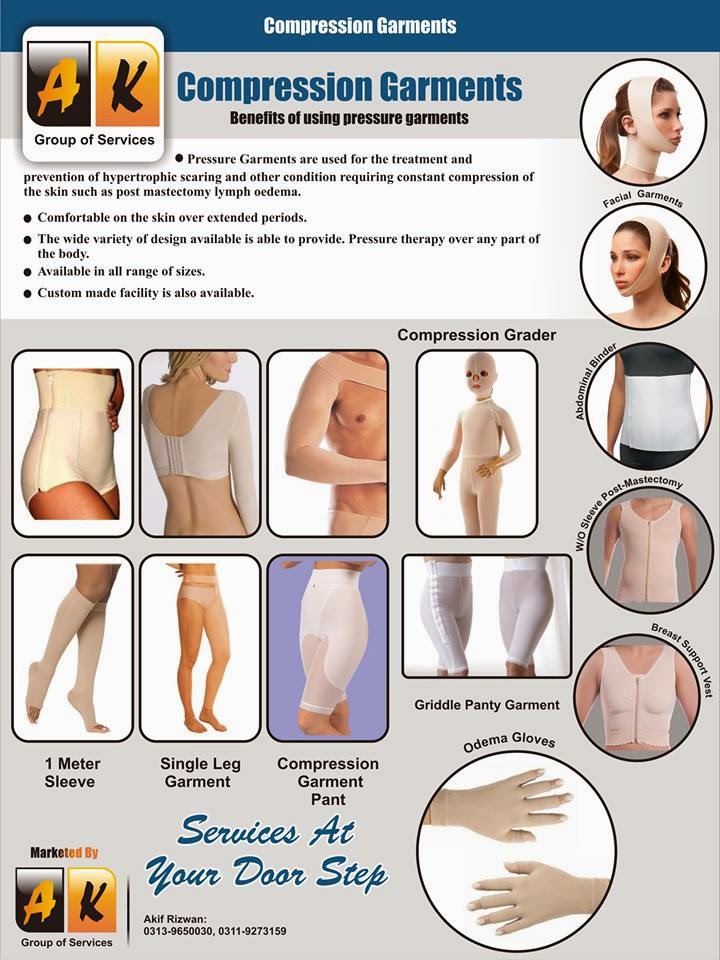
Abdominal Binder
Lots of
women love wearing a compression garment after their c-section. Without it they
feel unsupported and ‘loose’. A much praised benefit of a Abdominal Binder is that the firm support after the baby’s born gives them a
safe feeling.
An abdominal binder is
a special compression garment that you wear around your midsection. You may be
wondering why you would need to wear an abdominal binder after having a baby.
The reasons for wearing an abdominal binder are typically related to surgery or
childbirth – or sometimes, both! Maybe it seems like putting extra pressure on
your belly might even hurt. On the contrary, compression is a common technique
used to speed healing, often after surgery or after an injury like a sprained
ankle. Compression offers support to the area that is healing. Compression also
increases blood flow and reduces swelling, both of which are key components of
the healing process.
An abdominal binder is meant to be quite tight – though not so tight that you
can’t breathe or sit comfortably. Some abdominal binders are simple swaths of
thick fabric that you wrap around your belly area, securing the wrap with
velcro or a series of snaps. Other binders are more like a bodysuit that you
step into and pull up around you midsection.
Abdominal Binding to Speed Up the Healing Process
Abdominal Binder Post
Pregnancy
The purpose of an abdominal binder it to promote healing through compression. During pregnancy, your baby takes up an amazing amount of space inside your body. Your abdominal muscles are stretched to their limit, and your lower back muscles must compensate for the shift in your center of gravity. The growing baby pushes your internal organs out of the way as he grows and grow.
By the end of your
pregnancy, your stomach has been pushed up close to your heart! As anyone who
has had a baby knows, it takes some time before you return to your
pre-pregnancy shape. When your baby is born, she leaves behind an empty uterus
– and it takes approximately six weeks for this organ to shrink back to its
normal size. Likewise, your organs do not immediately return to
their pre-pregnancy
locations, either. An abdominal binder, however, can speed this process along.
Wearing an abdominal
binder as soon as possible after childbirth – no matter if you delivered
vaginally or with a c-section – works wonders for your healing process. You
should feel like your lower back is supported, even though your adbominal
muscles are not yet able to do this job on their own. The compression, along
with the natural after-birth contractions that you have, pushes your uterus
from the outside in, helping it find its pre-pregnancy shape and location. The
same is true for your other abdominal organs: compression can help your stomach
and intestines drop back into their previous position.
Muscle Support after Pregnancy
Binding your abdomen can also remind your abdominal muscles how to behave. Though you may not be consciously tightening your abs, the compression helps them snap back from being stretched to accomodate your baby. If you had a c-section, an abdominal binder is a must for your healing process. Compression over your incision will help reduce the pain that many women feel when they laugh, cry, or even roll over in bed. Wearing a compression garment will help your incision heal faster, too, because compression will increase blood flow to that area and help reduce the swelling around your incision.
There are so many
options for abdominal binders on the market today. The best products offer a combination
of comfort and support. The right abdominal binder should also be easy to use!
Panels in the front and back of the garment will support your midsection as you
heal.
A snug fit ensures
that the garment will not slip off, even as you care for you new baby and
resume your normal daily activities. A hook and eye closure makes it easy to
use the restroom without having to take the entire garment off, too! You can
put it on when you get out of bed in the morning and not think about it again
until you take it off at night. In fact, many women choose to wear the binder
24 hours a day – even while sleeping – to receive the maximum benefit from
abdominal compression!
At first glance, an
abdominal binder may seem like an unnecessary expense for postpartum women. But
the results you will see make the investment in your body and your health worth
every penny.
·
Abdominal surgical
binder for post-op rehab, muscle soreness or strains
·
Three, four or solid
panel design choices
·
Unisex
·
Made of latex-safe
elastic
Our Services at your Door Step..Home Delivery With Time Management
For more Details please contact to our respected officers
Deans Trade Center FF 356 Peshawar Cantt:
Contacts :
Manager Sales Akif Rizwan :+923139650030
Manager Marketing Khalid Iqbal +923149005932